References
Sausville, E. A. & Burger, A. M. highlighted the impact of human tumor xenografts in advancing anticancer drug development, showcasing the established strategies in Cancer Research, Volume 66, Pages 3351–3354.
Day, C. P., Merlino, G. & Van Dyke, T. explored the intricate landscape of preclinical mouse cancer models. Their findings reveal both potential and hurdles in the development process as discussed in Cell, Volume 163, Pages 39–53.
Holen, I. et al. provided an overview of in vivo models in breast cancer research, focusing on both advancements and future perspectives in Disease Models & Mechanisms, Volume 10, Pages 359–371.
Hidalgo, M. et al. discussed the emergence of patient-derived xenograft models as a promising platform for translational cancer research in Cancer Discovery, Volume 4, Pages 998–1013.
Hait, W. N. addressed the significant challenges in anticancer drug development in Nature Reviews Drug Discovery, Volume 9, Pages 253–254.
Johnson, J. I. et al. investigated the correlations between drug efficacy in NCI’s preclinical models and initial clinical trials in British Journal of Cancer, Volume 84, Pages 1424–1431.
Prinz, F. et al. analyzed the reliability of published data regarding drug targets in Nature Reviews Drug Discovery, Volume 10, Pages 712–712.
Whittle, J. R. et al. examined patient-derived xenograft models in breast cancer and their predictive capabilities in Breast Cancer Research, Volume 17, Article 17.
Yada, E. et al. discussed the applications and challenges of patient-derived xenograft mouse models in cancer treatment in Future Science OA, Volume 4, Article FSO271.
Shamseddin, M. et al. explored the effects of contraceptive progestins with androgenic properties on breast epithelial cell proliferation in EMBO Molecular Medicine, Volume 13, Article e14314.
Sflomos, G. et al. described a preclinical model for estrogen receptor alpha-positive breast cancer, emphasizing the epithelial microenvironment’s role in hormone response in Cancer Cell, Volume 29, Pages 407–422.
Duss, S. et al. created an estrogen-dependent model of breast cancer through normal human mammary epithelial cell transformation, observed in Breast Cancer Research, Volume 9, Article R38.
Scabia, V. et al. illustrated that estrogen receptor-positive breast cancers display patient-specific hormone sensitivities, relying on the progesterone receptor in Nature Communications, Volume 13, Article 3127.
Fiche, M. et al. demonstrated that intraductal patient-derived xenografts of estrogen receptor alpha-positive breast cancer reflect the histopathological spectrum and metastatic potential of human tumors in Journal of Pathology, Volume 247, Pages 287–292.
Sflomos, G. et al. found that lobular carcinoma cells in intraductal xenografts depend on their own extracellular matrix and LOXL1 in EMBO Molecular Medicine, Volume 13, Article e13180.
Abdolahi, S. et al. explored patient-derived xenografts (PDX) models, addressing their applications and challenges in cancer research in Journal of Translational Medicine, Volume 20, Article 206.
Carpenter, R. S. et al. investigated the infiltration of human immune cells in the spinal cord, affecting recovery post-injury in humanized mouse models as reported in Scientific Reports, Volume 9, Article 19105.
Zhao, Y. et al. developed a novel humanized mouse model simulating the human tumor microenvironment and immunotherapy in Gut, Volume 67, Pages 1845–1854.
Scherer, S. D. et al. presented an immune-humanized PDX model for estrogen-independent, hormone receptor-positive metastatic breast cancer in Breast Cancer Research, Volume 23, Article 100.
Dobrolecki, L. E. et al. reviewed the role of PDX models in both basic and translational breast cancer research in Cancer Metastasis Reviews, Volume 35, Pages 547–573.
Kostlan, R. J. et al. discussed clinically relevant humanized mouse models for metastatic prostate cancer, facilitating therapeutic evaluation in Molecular Cancer Research, Volume 22, Pages 826–839.
Yang, Y. et al. outlined the utility of humanized mouse models for preclinical cancer evaluation in Biotechnology and Bioengineering, Volume 121, Pages 835–852.
Henderson, B. E. & Feigelson, H. S. focused on hormonal carcinogenesis in Carcinogenesis, Volume 21, Pages 427–433.
Brisken, C. emphasized the importance of progesterone signaling in breast cancer, shedding light on a previously overlooked hormone in Nature Reviews Cancer, Volume 13, Pages 385–396.
Singh, R. R. & Kumar, R. discussed the influence of steroid hormone receptor signaling on tumorigenesis in Journal of Cellular Biochemistry, Volume 96, Pages 490–505.
Costa, A. R. et al. reviewed the sex bias in cancer incidence and outcomes in Trends in Endocrinology & Metabolism, Volume 31, Pages 785–799.
Manolagas, S. C. & Kousteni, S. presented insights on the non-reproductive actions of reproductive hormones in Endocrinology, Volume 142, Pages 2200–2204.
Gil, D. et al. established the link between dihydrotestosterone and increased bladder cancer risk in men found in Human Cell, Volume 32, Pages 379–389.
Godoy, G. et al. analyzed the impact of androgen and estrogen receptor signaling on bladder cancer dynamics in Bladder Cancer, Volume 2, Pages 127–137.
Chen, J. et al. detailed the role of the androgen receptor in bladder cancer pathogenesis in Nature Reviews Urology, Volume 20, Pages 560–574.
Li, Z. et al. emphasized the essential roles of Foxa1 and Foxa2 in liver cancer sexual dimorphism in Cell, Volume 148, Pages 72–83.
Zhang, L. et al. investigated the steroid axis contributions to male predominance in hepatocellular carcinoma in Cancer Letters, Volume 555, Article 216037.
Liu, J. et al. explored estrogen and estrogen receptor signaling pathways in thyroid cancer development in Frontiers in Oncology, Volume 11, Article 59347.
Derwahl, M. & Nicula, D. reviewed the role of estrogen in thyroid cancer in Endocrine-Related Cancer, Volume 21, Pages T273–T283.
O’Grady, T. J. et al. studied hormonal and reproductive factors’ associations with differentiated thyroid cancer risk among women in the International Journal of Epidemiology, Volume 53, Article dyad172.
Kelsey, J. L. & Horn-Ross, P. L. provided an epidemiological overview of breast cancer in Epidemiologic Reviews, Volume 15, Pages 7–16.
Chang-Claude, J. et al. evaluated age at menarche and menopause as breast cancer risk factors in the International BRCA1/2 Carrier Cohort Study, Cancer Epidemiology, Biomarkers & Prevention, Volume 16, Pages 740–746.
Colditz, G. A. et al. examined breast cancer risk according to estrogen and progesterone receptor status in Journal of the National Cancer Institute, Volume 96, Pages 218–228.
Travis, R. C. & Key, T. J. analyzed estrogen exposure and breast cancer risk in Breast Cancer Research, Volume 5, Article 239.
Villa, P. et al. presented a narrative review on hormone replacement therapy in post-menopausal women with gynecological cancer in Journal of Clinical Medicine, Volume 13, Article 1443.
Bull, J. R. et al. shared real-world menstrual cycle characteristics from over 600,000 cycles in NPJ Digital Medicine, Volume 2, Article 83.
Jänne, M. et al. studied human sex hormone-binding globulin gene expression in transgenic mice, detailed in Molecular Endocrinology, Volume 12, Pages 123–136.
van Weerden, W. M. et al. found that mouse and rat adrenal glands do not synthesize androgens in Life Sciences, Volume 50, Pages 857–861.
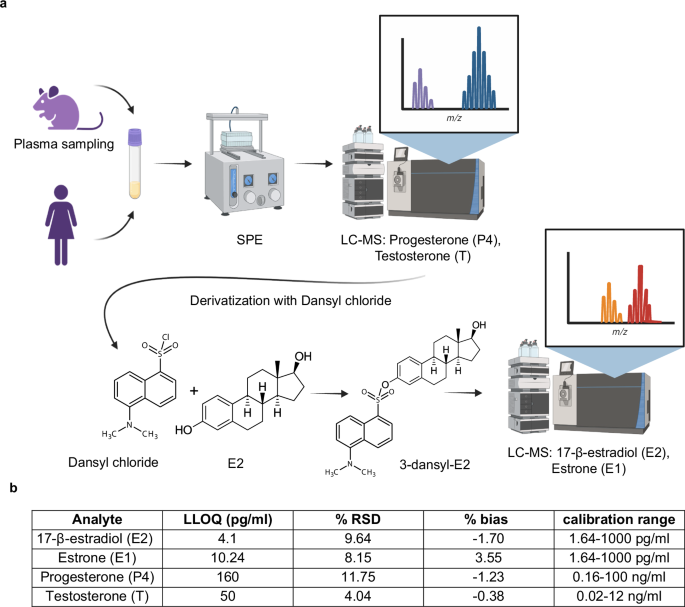
Nilsson, M. E. et al. developed a comprehensive method for measuring sex steroids in rodent serum, presented in Endocrinology, Volume 156, Pages 2492–2502.
Beery, A. K. & Zucker, I. discussed the implications of sex bias in neuroscience and biomedical research in Neuroscience & Biobehavioral Reviews, Volume 35, Pages 565–572.
Zheng, D. et al. reviewed sexual dimorphism in human cancer incidence in BMC Cancer, Volume 19, Article 684.
Clocchiatti, A. et al. provided insights on sexual dimorphism in cancer in Nature Reviews Cancer, Volume 16, Pages 330–339.
Auchus, R. J. discussed best practices for steroid assays and endocrinology for basic scientists in Endocrinology, Volume 155, Pages 2049–2051.
Handelsman, D. J. & Wartofsky, L. emphasized the importance of mass spectrometry in sex steroid assays as noted in Journal of Clinical Endocrinology and Metabolism, Volume 98, Pages 3971–3973.
Rosner, W. et al. discussed challenges associated with estradiol measurements in an Endocrine Society position statement published in Journal of Clinical Endocrinology and Metabolism, Volume 98, Pages 1376–1387.
Folkerd, E. J. et al. highlighted the need for caution interpreting plasma estrogen levels in breast cancer research found in Journal of Clinical Oncology, Volume 32, Pages 1396–1400.
Karashima, S. & Osaka, I. presented findings on the rapidity and precision of steroid hormone measurements in Journal of Clinical Medicine, Volume 11, Article 956.
Laszlo, C. F. et al. developed a high-resolution method for analyzing contraceptive progestins and steroids, published in Journal of Pharmaceutical and Biomedical Analysis, Volume 175, Article 112756.
Wang, Q. et al. detailed an ultra-high sensitivity analysis of estrogens using LC-MS for special populations in Journal of Steroid Biochemistry and Molecular Biology, Volume 162, Pages 70–79.
Cagnet, S. et al. explored estrogen receptor alpha’s domains and their cell population-specific roles in mammary epithelium in Nature Communications, Volume 9, Article 4723.
Ke, Y. et al. created a sensitive and robust LC-MS/MS method for quantifying androgen- and estrogen-related steroids in postmenopausal serum in Journal of Steroid Biochemistry and Molecular Biology, Volume 144, Pages 523–534.
Nelson, R. E. et al. presented a liquid chromatography-tandem mass spectrometry assay for simultaneous measurement of estradiol and estrone in human plasma in Clinical Chemistry, Volume 50, Pages 373–384.
Vitku, J. et al. compared derivatized vs. non-derivatized LC-MS/MS techniques for analyzing estrogens in human plasma in Ecotoxicology and Environmental Safety, Volume 260, Article 115083.
Wood, G. A. et al. found links between circulating hormones and estrous stage with cellular and stromal remodeling in murine uterus in Reproduction, Volume 133, Pages 1035–1044.
Toran-Allerand, C. D. et al. questioned whether 17α-estradiol acts as a brain-active estrogen in Endocrinology, Volume 146, Pages 3843–3850.
Sims, N. A. et al. studied estrogen receptors’ roles in bone remodeling variations between genders in Bone, Volume 30, Pages 18–25.
Lindberg, M. K. et al. characterized estrogen receptor specificity affecting the skeleton in female mice in Journal of Endocrinology, Volume 171, Pages 229–236.
Caldwell, A. S. L. et al. detailed reproductive, metabolic, and endocrine features of polycystic ovary syndrome in female hyperandrogenic mouse models in Endocrinology, Volume 155, Pages 3146–3159.
Handelsman, D. J. et al. discussed ultrasensitive serum estradiol measurement by LC-MS in postmenopausal women and mice in Journal of Endocrine Society, Volume 4, Article bvaa086.
Weng, Y. et al. analyzed testosterone and dihydrotestosterone levels in mouse tissues via liquid chromatography-electrospray ionization-tandem mass spectrometry in Analytical Biochemistry, Volume 402, Pages 121–128.
Kratz, A. et al. compiled normal reference laboratory values in New England Journal of Medicine, Volume 351, Pages 1548–1563.
Verdonk, S. J. E. et al. established estradiol reference intervals in men and women across menstrual cycles in Clinical Chimica Acta, Volume 495, Pages 198–204.
Stricker, R. et al. determined detailed reference values for luteinizing hormone, follicle-stimulating hormone, estradiol, and progesterone during menstrual phases in Clinical Chemistry and Laboratory Medicine, Volume 44, Pages 883–887.
de Wit, A. E. et al. examined the relationship between plasma androgens and depression in a large cohort of women, reported in Translational Psychiatry, Volume 11, Article 124.
Kyriakopoulou, L. et al. developed a rapid mass spectrometric method for measuring steroid hormones along with CALIPER pediatric reference intervals in Clinical Biochemistry, Volume 46, Pages 642–651.
Wooding, K. M. et al. measured estradiol, estrone, and testosterone in postmenopausal human serum via isotope dilution LC-MS without derivatization in Steroids, Volume 96, Pages 89–94.
Faqehi, A. M. M. et al. found that estrogen derivatization enhanced analysis specificity and sensitivity in human plasma through LC-MS/MS, as reported in Talanta, Volume 151, Pages 148–156.
Li, X. & Franke, A. A. improved estrogen metabolite profiling through orbitrap LC/MS, published in SI Measurement: Estrogen Exposure Metabolism, Volume 99, Pages 84–90.
Kalra, S. P. & Kalra, P. S. reviewed the interrelationships among estradiol, progesterone, and LH during the rat estrous cycle in Endocrinology, Volume 95, Pages 1711–1718.
Denver, N. et al. assessed current strategies for quantifying estrogens in clinical research in Journal of Steroid Biochemistry and Molecular Biology, Volume 192, Article 105373.
Shifren, J. L. et al. discussed transdermal testosterone treatment effects in women post-oophorectomy in New England Journal of Medicine, Volume 343, Pages 682–688.
Flores, A. et al. investigated the effects of ovariectomy and adrenalectomy on steroid levels, depending on surgical timing in Reproductive Biology and Endocrinology, Volume 6, Article 48.
Qureshi, R. et al. described the opposing roles of pre- and postmenopausal estrogens in obesity-linked mammary inflammation and breast cancer in Cell Metabolism, Volume 31, Pages 1154–1172.
Shaw, N. D. et al. provided evidence for estrogen’s direct influence on gonadotropin secretion in women in Journal of Clinical Endocrinology and Metabolism, Volume 95, Pages 1955–1961.
Glidewell-Kenney, C. et al. demonstrated that nonclassical estrogen receptor alpha signaling mediates negative feedback in female mice reproductive systems in Proceedings of the National Academy of Sciences, Volume 104, Pages 8173–8177.
Knedla, A. et al. utilized osmotic minipumps in SCID mouse models for rheumatoid arthritis treatment as reported in Annals of the Rheumatic Diseases, Volume 68, Pages 124–129.
Tan, T. et al. introduced programmable technology for drug delivery in iPRECIO® Micro Infusion Pump in Frontiers in Pharmacology, Volume 2, Article 44.
Itzhaki, E. et al. discussed tumor-targeted nanocapsules for personalized cancer therapy in Advanced Therapy, Volume 6, Article 2200337.
Moskovits, N. et al. explored the synergistic effects of Palbociclib combined with Sunitinib in patient-derived xenograft models of various cancers in Cancer Letters, Volume 536, Article 215665.