In recent years, the use of modern contraceptives—methods that do not involve surgical procedures like tubectomies or vasectomies—has surged globally. According to the World Health Organization, the number of women utilizing modern contraceptive methods rose from 663 million in 2000 to 851 million by 2020. Projections indicate an additional 70 million women are expected to adopt these methods by 2030.
Modern contraceptives encompass a range of hormone-based options, including progestogen-only pills (often referred to as mini-pills), combined oral contraceptives (the pill), and contraceptive patches. In India, the National Family Health Survey (NFHS) shows a significant increase in the use of modern contraceptives across nearly all states and union territories, with the national Contraceptive Prevalence Rate (CPR) climbing from 54% to 67%.
While hormonal contraceptives empower women with greater autonomy over their reproductive choices, their impact on women’s health, particularly regarding side effects, remains inadequately studied and varies among individuals.
Hormones and Mental Well-Being
According to Sapna Raina, a senior consultant in obstetrics and gynecology at Narayana Health City in Bengaluru, the mental health ramifications of contraceptives are closely tied to the hormones they release, chiefly estrogen and progesterone. “Hormonal contraceptives affect not only physical but also psychological health in women,” she notes.
Estrogen significantly influences brain neurotransmitters such as serotonin and dopamine, which play a crucial role in regulating mood and emotional stability. “Estrogen likely has a more profound effect than progesterone, potentially leading to mood swings, irritability, anxiety, and depression,” she explains.
Research suggests that the combined oral contraceptive pill tends to be associated with more pronounced psychological effects compared to progesterone-only pills; nevertheless, mini-pills may still lead to mild side effects including fatigue and mood fluctuations.
Dr. Raina cautions that for some women, especially those with a prior history of anxiety or depression, the use of hormonal contraceptives can exacerbate their mental health issues. She also mentions that contraceptives administered via injection, like Depo-Provera, can have similar psychological impacts. Conversely, the intrauterine hormonal device (IUD), such as Mirena, tends to have a localized effect, thus being less likely to trigger widespread mental health concerns, although mood variations are still possible.
Physical Health Considerations and Recommendations
The ramifications of hormonal contraceptives extend beyond mental health. Dr. Raina points out severe physical risks, such as thromboembolic events—blood clots that can migrate to crucial organs like the lungs or brain, posing the risk of pulmonary embolisms or strokes.
“Long-term use of combined oral contraceptive pills may heighten a woman’s susceptibility to blood clots, which can dislodge and jeopardize her brain or lungs,” she warns. She emphasizes the importance of women on hormonal birth control to remain proactive in maintaining their health through proper hydration and regular physical activity.
A Variety of Contraceptive Options
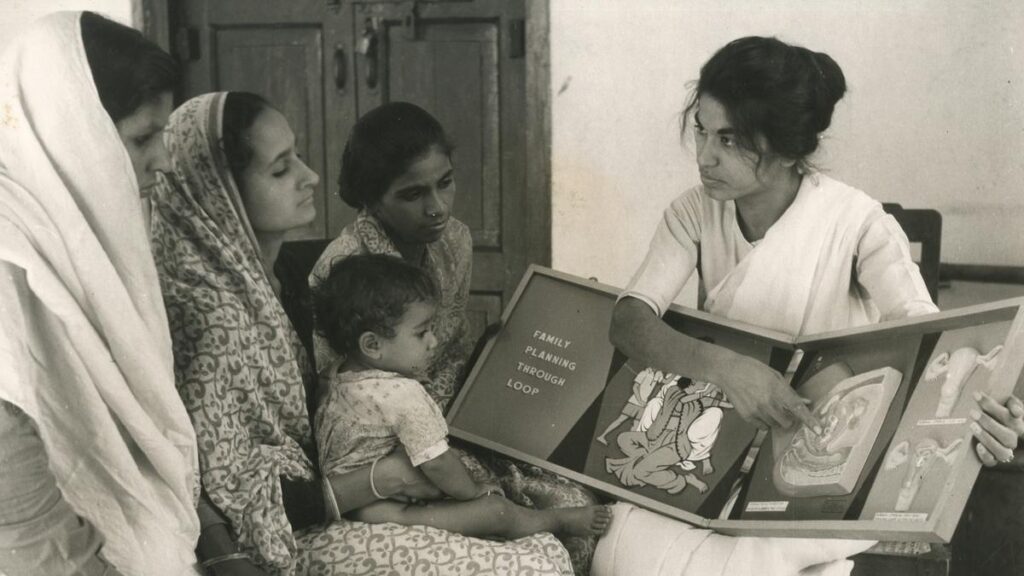
T.K. Shaanthy Gunasingh, president of the Chennai Menopause Society, stresses the responsibility of healthcare providers to offer women a comprehensive range of contraceptive options rather than a one-size-fits-all approach. Educating women about long-acting reversible contraceptives (LARCs), such as intrauterine devices, which can be effective for up to a decade but can also be removed earlier if desired, is essential. Unlike daily hormonal pills, these options provide much-needed flexibility.
Dr. Gunasingh highlights that although healthcare professionals may be aware of the complete spectrum of contraceptive choices, not all women have the same level of understanding. “We must engage women in discussions about all of their options, clarifying how each method operates and supporting their choices. It’s crucial to initiate dialogue about contraception even during pregnancy, so by the time a woman gives birth, she has a clear plan in mind. While it’s important to respect her decisions if she changes her mind, being informed is key,” she states.
“Ensuring that women have a range of choices and receive personalized care is vital for making informed decisions about their reproductive health; they should never feel confined to one method if it does not suit them,” she insists.
Raising Awareness
While contraceptives play a pivotal role in family planning, experts encourage a holistic approach to healthcare that not only provides contraceptives but also educates women about possible mental and physical side effects. Government initiatives distributing oral contraceptive pills like Mala D and Mala N at no cost at health centers aim to ensure access for women across various socioeconomic backgrounds. Dr. Raina emphasizes the need for cautious prescription practices and responsible distribution to avert misuse.
Experts agree that each individual’s body reacts differently to contraceptives; if one method doesn’t work for someone, alternatives are available, but it is crucial to have conversations about all possible options.
N. Syamala, senior consultant in obstetrics and gynecology at SP Fort Hospital and Ananthapuri Hospital in Thiruvananthapuram, underscores that contraceptives can serve purposes beyond birth control, such as treating specific medical issues like heavy menstrual bleeding or hormonal imbalances. However, she cautions that emergency contraceptive pills, such as the I-pill, are not intended for routine use.
Dr. Gunasingh concludes by stating, “Contraception should provide women with peace of mind, not only in preventing pregnancy but also in fostering a sense of control over their reproductive health. With adequate information and medical guidance, women can make choices that align best with their bodies and lifestyles.”